Mother was a smart, resourceful, attractive, tactless, competitive and practical person. She was what was called a girl with promise, and if times were different, she might have fulfilled that promise. She had wanted to write and paint, but instead she married and had children. She worked for a while before marriage but as soon as my father was making good money, as they called it, she quit, fulfilling an American 1950s ideal – women whose husbands do well will stay at home with their children, content to be wives and mothers. Mother was not, and she was angry, and for that I don’t blame her.
When many Americans in the postwar period moved to the suburbs, my parents did also, from the family’s comfortable apartment in Brooklyn to a house on Long Island, one partly of their own design. It’s where I grew up from the age of five. Mother hadn’t wanted to move to the suburbs, but my father insisted on the American dream. It was, in my opinion, a nightmare for Sophie, the city girl used to speed, museums, parks, taxis, subways – she didn’t like having to drive – and sidewalks, which our street didn’t have, ever. It was all forest with a swamp at the end of it.
My parents retired to Florida, where she had never wanted to live; again, my father insisted. With her husband dead in 1984, alone in Florida Mother was miserable and bored, but with the help of my Manhattan sister, about three years after my father died, Mother moved to Manhattan. My sister found a great apartment for her on Second Avenue and Twenty-third Street. It was convenient, central, and, because she didn’t need to get anywhere fast, crosstown buses were fine.
Her daytime doorman, Ray, told me that, in her first month, he thought Mother couldn’t adjust to city life. He thought it would be too hard for her. After another month, Ray said she was doing fine, and they developed a sweet friendship. Ray was a very kind man, avuncular with her, though she was years older.
Almost seventy-nine, Mother discovered a new life, became reacquainted with the city, an old friend – they had met in school when they were twelve years old – watched movies at MOMA, saw plays, and walked everywhere. Mother was Kazin’s walker in the city, she loved walking. In Florida and the suburbs walking was eccentric.
Mother had seven and a half good years as an independent character.
Then, at eighty-six and a half, Mother showed unusual behavior, symptoms of trouble.
I’d been away almost four months, from September to mid-December 1994, as a visiting writer in the English and American Literature department at the University of Sussex, Brighton, England. During those months, we had no contact. I returned in December, and Mother and I met for breakfast at our usual Polish café. I entered, saw Mother seated at our usual table, and approached, but she didn’t look up. She was staring vacantly at the tabletop, and didn’t greet me. I said, ‘Hi, Mom, I’ve been away, aren’t you happy to see me?’ She glanced up. ‘Sure,’ she said, indifferently. Distant, hair disheveled, she appeared out of sorts, even depressed. Mother was not a depressive; for one, she expressed anger frequently. Her affect now was atypical, puzzling.
We walked uptown to her apartment on Twenty-third Street. On the corner of Thirteenth Street and Second Avenue, we passed what appeared to be a homeless man. Mother commented, ‘He’s waiting for someone.’ Her interpretation was a kind of identification with him or a projection, and unusual from her mouth. Later, I thought: she’s waiting for her husband, my father.
That night or the next morning I phoned one of my two older sisters, I forget which one, probably the New York one. She had noticed the change, also.
Out of the blue, Mother was desperately sick, and it happened to our entire, small family. Each day, in the beginning, the first year or two, seemed urgent. How to handle her condition, what was the right course to help her, what could be done differently and better.
I found all of my diaries for those years but not 1995, the first year of her as-yet-unknown condition. Mother’s calendar for 1995 had some missing months, March–October, and by November she no longer kept her calendar. I did, or one of my sisters. Later, her longtime caregiver took over, writing in doctors’ and other appointments, physical therapy days. I used the diaries to remember. Some events are sharply in focus, scenes manifest in good detail. What people said, also, whole sentences, responses, queries, they return. Most is lost, especially the moments between, the preludes to bigger events or main events, like Mother’s surgeries.
First, we noticed that Mother behaved strangely, she was not herself. I can’t remember how we took our first steps, moves toward finding out what was wrong. Those decisions are just lost. We sisters knew Mother needed an accurate diagnosis, urgently. I don’t recall who made the first appointment, with whom. Mother had already had an MRI with her longtime internist. He believed her brain looked normal for an aging brain. He thought the ventricles were normally sized.
A first neurologist, to whose office I brought her, was convinced from the same MRI that she had Alzheimer’s. I received a phone call from him – he didn’t want to tell me in front of Mother, luckily. I was home, sitting in the kitchen, and he pronounced that awful death sentence. Then he said, ‘But bring her back in six months, and we’ll see.’ That didn’t happen.
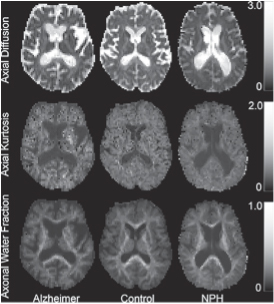
Sample parametric maps for patients with Alzheimer’s disease (left), healthy controls (center), and those with normal pressure hydrocephalus (right)
Mother’s symptoms didn’t correlate to a diagnosis of Alzheimer’s – the onset of her illness was not incremental; from one day to the next, she showed impairment, her symptoms were not intermittent. She changed significantly or drastically, and the change was consistent.
There were differences among us sisters as time went on. Mother’s behavior was erratic and difficult to diagnose, but primarily we stuck to the empirical reality that Mother’s condition came on fast, unlike Alzheimer’s.
I’m just a medical-science observer, interested in sickness, so-called wellness, cures, trials, placebos, successful and failing bodies. I read medical newsletters, and writers such as Rachel Aviv, Atul Atawande, Siddhartha Mukherjee, and Jane Brody. I read most of the Times Science section. Learning that Mother’s MRI would be interpreted differently by three of the four doctors floored me. Two agreed, the other two differed in their analyses and also from each other. An MRI is not a blueprint; it doesn’t tell the brain’s secrets.
No certainty in reading the brain and, like reading any text, an MRI requires interpretation, which a doctor decides based on what any one of us brings to any object: education, training, belief, subjectivity. In a sense, perception is immune to objectivity, perception is a disposition: one is disposed to see this way or that, which made finding a conclusive diagnosis for Mother’s condition difficult.
Inevitably, patient advocates or family go up against medical experts. In medicine, as in most fields, differences in theory and technique occur. A doctor’s expertise is not inviolable. Doctors may even cover uncertainties and inadequacies, their lacks, with clever obfuscation. A patient hopes, expects, that doctors will be honest brokers and admit to their educated guesses, saying: ‘This may not be the right diagnosis or treatment, but I believe this is what needs to be done.’ A patient hopes the doctor might, in complicated cases, present several options, expatiating on their advantages and disadvantages. ‘Of these options, I’d do this,’ a doctor might say. But patients want to believe there is one best treatment. Often there isn’t.
Any opinion or theory provided by the family to the doctor is usually where the doctor starts – analyzing, hypothesizing, speculating, diagnosing. Giving your conclusions first is a mistake. Medical reporting is a narrative, the order of telling influences doctors’ first moves and their interpretations. An advocate must be wary of diagnosing symptoms; instead, present evidence or problems chronologically, without interpretation, as best you can. When this happened, what occurred before . . . This isn’t easy. Believe me, your empirical observations and impressions matter, but they might not be or shouldn’t be answers.
On the other hand, and there are many, passivity hinders. Caregivers might have to get in the doctors’ faces, querying their decisions, prescriptions, even annoying them. Doctors are not gods, though some act that way. Some hate being questioned. Some have no time to listen. Some are fine. Many do a good job. They can fire you, I guess, but we never had that experience. More likely, you will need to fire them. Do what you must to get what you need – careful attention, a listener (you also must listen well), genuine thoughtfulness, candor, and truthfulness.
Image © Drew Morton

This is an excerpt from Mothercare by Lynne Tillman, out with Peninsula Press in the UK and Soft Skull Press in the US.







